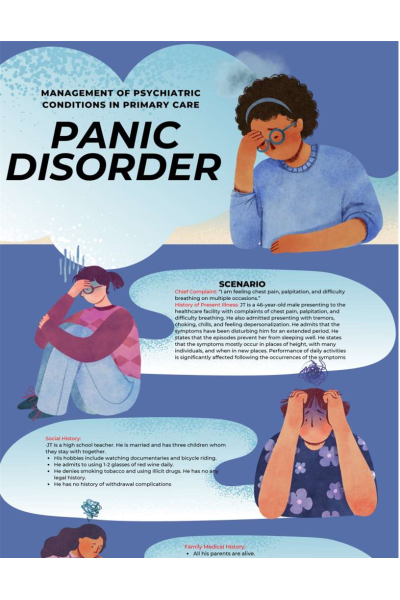
SCENARIO
Chief Complaint: “I am feeling chest pain, palpitation, and difficulty
breathing on multiple occasions.”
History of Present Illness: JT is a 46-year-old male presenting to the healthcare facility with complaints of chest pain, palpitation, and difficulty breathing. He also admitted presenting with tremors, choking, chills, and feeling depersonalization. He admits that the symptoms have been disturbing him for an extended period. He states that the episodes prevent her from sleeping well. He states that the symptoms mostly occur in places of height, with many individuals, and when in new places. Performance of daily activities is significantly affected following the occurrences of the symptoms.
Social History:
·JT is a high school teacher. He is married and has three children whom they stay with together.
His hobbies include watching documentaries and bicycle riding. He admits to using 1-2 glasses of red wine daily.
He denies smoking tobacco and using illicit drugs. He has no any legal history.
He has no history of withdrawal complications......... Continue
| Instituition / Term | |
| Term | Uploaded 2023 |
| Institution | Chamberlain |
| Contributor | Nina |