NR 601 Week 8 Final Exam Textbook Questions with Answers
-
$60.00
| Institution | Chamberlain |
| Contributor | Sharoon |
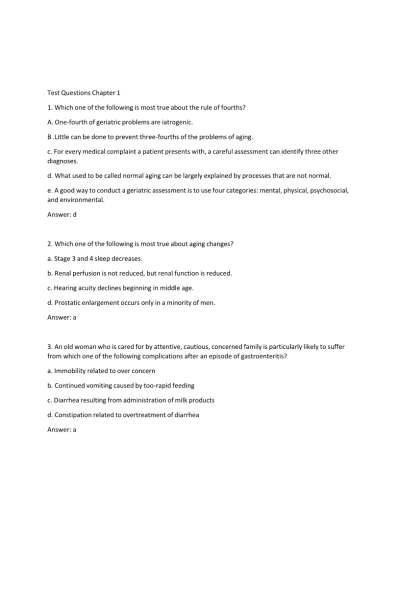
Test Questions Chapter 1
- Which one of the following is most true about the rule of fourths?
- Which one of the following is most true about aging changes?
- An old woman who is cared for by attentive, cautious, concerned family is particularly likely to suffer from which one of the following complications after an episode of gastroenteritis?
- Which one of the following is most true about psychological aging?
- Of the following conditions, which one is most common and most often preventable?
Test Questions Chapter 4
- An 86-year-old female comes to your office for a wellness visit. Her blood pressure is 125/70 mmHg, pulse 69 beats per min, and respiratory rate 18 breaths per min. She is well appearing and reports she is up to date on her routine vaccinations. She introduces her partner of 35 years whom she would like to make medical decisions for her in case she becomes unable to make decisions for herself. She reports that she and her partner are not married. She asks if she needs any further documentation to ensure her goals of care are followed. Which one of the following would be the most appropriate recommendation for this patient and her partner?
- An 81-year-old transgender female with history of depression and hyperlipidemia presents to your clinic for routine care. She endorses a history of smoking, currently smoking 1 pack per day, and occasionally drinks a glass of wine, although she denies illicit drug use. She reports she takes atorvastatin 20 mg and subcutaneous estrogen therapy. Which of the following is the most important next step in this patient’s primary care?
- An 84-year-old male with history of stroke without residual deficit, systolic heart failure, and type 2 diabetes presents to clinic for follow-up. He is independently living in a retirement community and still works part time on a golf course. He currently takes aspirin 81 mg, metoprolol tartrate 25 mg BID (twice a day), furosemide 20 mg BID, and lisinopril 10 mg daily. He reports his last colonoscopy was 8 years ago, with no abnormality. He reports he is sexually active with men and women, engaging in receptive oral, receptive anal, and penetrative sex. He states he has had over three sexual partners in the last year with intermittent condom use. What sexually transmitted infection testing should be offered?
Test Questions Chapter 5
- The US Advisory Committee on Immunization Practices and the Centers for Disease Control currently recommend which one of the following?
- Healthcare providers should recommend that older adults engage in which one of the following?
- Guidelines for the primary prevention of stroke recommend that aspirin be used in which one of the following?
- Even though older adults are less likely to get counseled for smoking cessation, they have which one of the following?
Test Questions Chapter 6
- Which of the following is true about cultural humility?
- Racial disparities have been a part of US healthcare for many decades. How might this impact the expectations of older Black Americans?
- Dementia is a relatively common condition in the geriatric population. It becomes more common as people age. Which is the most appropriate description of “personhood” as it relates to people with dementia?
- Immigrant families bring cultural traditions into healthcare decisions. With regard to older adults, which of the following is true?
Test Questions Chapter 8
- Which of the following statements concerning advance directives is true?
- The following are components of the open disclosure of medical error, except:
- Mrs. Gloth is an 84-year-old woman whom you are admitting to the nursing home. Her son takes you aside and tells you that she has metastatic ovarian cancer but has not been told the diagnosis. He asks that you not tell her, because she would “lose all hope and die.” Which of the following is an appropriate response?
- Dr. Smith is obtaining informed consent from Mr. Jones to perform a colonoscopy, because the patient had blood in his stool and Dr. Smith is concerned that this might indicate the presence of carcinoma of the colon. Mr. Jones is able to recite back to Dr. Smith what a colonoscopy is, how it is done, and that a colonoscopy is performed to look for cancer. He then tells Dr. Smith that he is refusing the procedure; he knows he does not have cancer because he has not experienced any bleeding. Of the following required elements for Mr. Jones’s decision-making capacity, which is impaired?
- George Hall is a 91-year-old man visiting his physician to receive the results of a recent computed tomography scan of his abdomen. He is cognitively intact and still works 2 days a week. He is accompanied by his daughter Eleanor. She takes the doctor aside before the appointment and says, “Please do not tell my father any bad news. It would just kill him.” If the physician were to agree, which ethical principles might this violate?
- Lenore White is an 80-year-old woman who smokes two packs of cigarettes per day. She is hospitalized for pneumonia because she has presenting symptoms of cough and fever. On her second day of hospitalization, she asks the nurse to please wheel her outside so she can smoke a cigarette. The nurse feels uncomfortable agreeing to this and speaks to her clinical nurse manager. What two ethical principles are in conflict?
- Ms. Greta Thornberg is an 88-year-old woman admitted to the hospital with a diagnosis of squamous cell carcinoma of the lung with metastases to liver. She has signed a POLST indicating that she would like no limitation on life-sustaining measures, including resuscitation, artificial feeding, antibiotics, and hydration. On the second day of her stay, she sustains a stroke, resulting in global aphasia and hemiparesis. As her clinician, in addition to instituting appropriate medical management, you contact her healthcare agent and:
Test Questions Chapter 9
- Which of the following statement about community-based services is true?
- Which sentence completion is false? The Veterans Health Administration:
- When a Medicare beneficiary with only traditional Part A and Part B coverage is admitted to the hospital, what will he or she will have to pay out of pocket?
- Since passage of the ACA in 2010, the following are true about payments changes except:
- All of the following about the Medicare Part D prescription medication benefit plan are true except:
- All of the statements about Medicare are true except:
- All of the statements about Medicaid are true, except:
Test Questions Chapter 12
- Mr. B is an 82-year-old enrolled in your primary care clinic panel. His medical history includes moderate dementia and probable Alzheimer disease. He requires cues to bathe and dress but is otherwise independent in his activities of daily living. He cannot manage his medications and does not drive. His wife is his primary caregiver and has been providing 24-hour care supervision since he was found wandering outside by their neighbors. During your visit today, she admits that she is “feeling stressed” and at times “overwhelmed” with her caregiving responsibilities. She wants to know what options are available to help support her taking care of him. All of the following would be appropriate for Mr. B except:
- Which of the following is true about the primary functions and duties of the skilled nursing facility medical director?
- Which one of the following is most true of the capacity to make medical decisions?
- Which one of the following is most true about the staffing of a typical nursing home?
Test Questions Chapter 15
- A 75-year-old man with lung cancer metastatic to the bones is receiving hospice care in his home. His predominant symptom is nociceptive and neuropathic right chest wall pain caused by a fourth rib metastasis. In recent days he has experienced a dramatic increase in his pain, and hospice staff have titrated his pain regimen to gabapentin 900 mg three times daily, extended release morphine 100 mg three times daily, and immediate release morphine 30 mg every 2 hours as needed. The hospice nurse calls you to ask about next steps, and reports that he is still in severe pain but is now nonverbal, and his family is struggling to administer his medication orally because of his somnolence. The patient’s family is exhausted. What is the best next step to assure the patient’s comfort?
- An 85-year-old woman with congestive heart failure, end-stage chronic obstructive pulmonary disease, chronic kidney disease stage 4, and frailty is brought to your office for a routine appointment. She has preserved cognition and her last Mini-Mental State Examination was 26. Affect is normal, and she has no history of depression. She has a loving and supportive family with whom she lives. During the visit, she shares that her quality of life is no longer acceptable, and asks about options to hasten the end of her life. Which of the following means of hastening death is legal throughout the United States?
- A 78-year-old woman with atherosclerotic cardiovascular disease (ASCVD), peripheral vascular disease, and a history of transient ischemic attacks s/p carotid endarterectomy is seen as part of an annual wellness visit. She is advised to create an advance directive but declines, saying “I don’t know who to pick” for a healthcare agent. Which one of the following is a necessary characteristic of a healthcare agent?
Test Questions Chapter 17
- A 67-year-old female with a history of congestive heart failure and myocardial infarction is admitted to the hospital because of increasing altered mental status and decreased arousal over the last week. Physical examination reveals a confused woman with right lower lobe crackles and a pulse oximetry of 86% on room air. While you are interviewing the patient, she is irritable, paranoid, and inattentive, which her family tells you is out of character. You notice waxing and waning in her alertness and impaired short-term memory during your examination. Which one of the following features present in this patient best distinguishes delirium from depression or dementia?
- A 72-year-old man with colonic diverticulosis was admitted to the hospital with gastrointestinal bleeding and abdominal pain. He underwent colonoscopy under conscious sedation using fentanyl and midazolam. The following day, the patient was positive on the Confusion Assessment Method performed by the geriatric consultation services. Presence of delirium in this patient predisposes him to all of the following except:
- A 78-year-old male who resides at a nursing home has Lewy Body dementia, frequent falls, visual hallucinations, and sleep disturbances. He is transferred to your hospital with poor oral intake and confusion of 3 days duration. Physical examination reveals a thin man with dry mucous membranes, tachypnea, tachycardia, and confusion. To reliably identify delirium in this patient in a time-efficient manner (<5 minutes), what will be your instrument of choice?
- An 84-year-old woman complains of nausea and vomiting for the past 3 days. She has a history of multiple abdominal surgeries, adhesions, and recurrent hospitalizations for partial small bowel obstruction. She has visual and hearing impairment and is currently taking oxybutynin for neurogenic bladder. You recognize she is high risk for development of delirium. Interventions that may prevent the onset of delirium among older adult hospitalized patients include all of the following except:
- A 78-year-old man with multiinfarct dementia, chronic kidney disease, congestive heart failure, and uncontrolled hypertension was hospitalized with a heart failure exacerbation. He was initially treated with diuretics and salt restriction and his condition stabilized. On day 3 of his hospital stay, he developed confusion, restlessness, and combativeness. Utilization of sitter, redirection, calming music, and reassurance are unsuccessful. When safety of the patient and staff are in jeopardy and nonpharmacologic approaches have failed, which of the pharmacologic agents would be the best choice for treating the agitation associated with his delirium?
Test Questions Chapter 18
- 1.A 69-year-old female presents to your office for routine primary care. Her elder sister was recently diagnosed with Alzheimer disease, and she wonders what steps she can take to reduce her own risk of developing dementia. Which of the following statements about the prevention of dementia is true?
- A 78-year-old male was recently diagnosed with Alzheimer disease. He scored 23/30 on his Montreal Cognitive Assessment chap21 (MoCA) and his clinical presentation is consistent with mild disease. He returns to clinic with his family to discuss possible initiation of pharmacotherapy. You consider beginning donepezil 5 mg daily for 4 weeks, with a plan to increase to 10 mg daily if he tolerates the lower dose. Which of the following is not a common side effect of donepezil?
Test Questions Chapter 19
- The remission rate of depressed patients who are 65 years and older to initial antidepressant treatment is:
- Which of the following groups has the highest rate of suicide in older adults?
- Which of the following is not a risk factor for late-life depression?
- Which of the following is not a side effect of selective serotonin reuptake inhibitors in older adults?
- You want to start pharmacologic treatment for depression in an older patient who is taking numerous medications. You are concerned about drug–drug interactions. Which of the following antidepressants is the least likely to cause such an interaction?
Test Questions Chapter 21
- Randall Johnson, an 80-year-old man with a history of high blood pressure and hypothyroidism, presents to your office with ongoing dizziness. He feels it has worsened since the summer months began. He states it is worst when he gets up from his chair on his front porch to stand or when he is working in his garden. If he stands still for a few minutes, the dizziness typically resolves on its own. If he tries to move too quickly, he has felt like he may pass out, but has not yet done so. He denies changes in vision or hearing. He has had no recent changes in his medication. On examination today, he is a frail- appearing older man in no acute distress. Vitals show a blood pressure of 118/71 mmHg with a pulse of 55 beats per minute. Heart and lung exams are benign. What is the most likely cause of his dizziness?
- Joyce Mitchell is a 73-year-old frail female with a history of frequent falls, who presents with rapid onset of nausea, vomiting, sweating, and horizontal nystagmus. She also reports hearing loss in the right ear. After testing and further questioning, you diagnose the patient with vestibular neuritis. What is the best initial course of treatment?
- Pedro Lopez is an 89-year-old male who presents to you with the complaint that he continuously experiences the feeling that a fall is imminent. He appears comfortable when seated, but is notably unsteady and imbalanced when erect, walking with a broad-based gait. Which of the following is not a standard treatment modality for this condition?
Test Questions Chapter 23
- Which of the following is true about tolterodine?
- An 82-year-old man, Mr. A, complains of worsening nocturia, occurring four times per night. His other lower urinary tract symptoms are slow stream, occasional urgency, and urgency-related leakage once weekly. Medical problems include poorly controlled hypertension, diastolic heart failure, hyperlipidemia, osteoarthritis, and prediabetes. His medications include lisinopril 20 mg daily, metoprolol succinate 75 mg daily, atorvastatin 10 mg daily, metformin 500 mg twice daily, hydrocodone-acetaminophen as needed, and aspirin 81 mg daily. Amlodipine 5 mg daily was recently added by his cardiologist. On review of systems, Mr. A complains that nocturia is causing daytime fatigue, and he is more constipated.
- Physical examination is notable for blood pressure 162/83 mmHg, heart rate 60 beats per minute, clear lungs, soft abdomen, enlarged prostate, and 21 pretibial edema. Your next step in management should be:
- The daughter of a 79-year-old woman notes that her mother, who has dementia and lives with her, is wetting herself when she attends her new day program. Program staff have requested that “something be done” as she is requiring a clothes change nearly every time she is there. She cannot describe the circumstances of leakage, saying “it just comes.” Leakage is uncommon at home. Her medications include donepezil and acetaminophen. Physical examination is normal. Initial treatment approach will require intervention by which of the following?
- Ms. J, who is 82 years old, complains of urine leakage while playing golf. This has gotten worse over the past year, and she rarely makes it through nine holes without feeling like she needs to “run into the bushes and go.” Leakage is usually small volume, but causes her extreme embarrassment because she is afraid she will smell of urine. She has tried limiting caffeine in the morning before she golfs and avoiding drinking water while playing, to no effect. She also tried “those Kegler” exercises in the past without success. Which of the following is the most appropriate recommendation for Ms. J?
Test Questions Chapter 29
- Which of these is true regarding the relationship of frailty with cognition?
- Which of these clinical vignettes are not part of the Fried frailty paradigms?
- Which of these statements about frailty are false?
- John P. is an 81-year-old male with extensive cardiac history, including three vessel coronary artery bypass graft when he was in his 60s, hypertension, diabetes mellitus, osteoarthritis, sciatica, and progressive macular degeneration. His vitals today are blood pressure 146/86 mmHg, heart rate 67 beats per minute, respiratory rate 21 breaths/min, and temperature 98.7° F. He is here with his only son and has been living in an assisted living since his wife died 3 years ago. His Montreal cognitive assessment (MoCA) 1 month ago was 23/30. He has no advance directive in the chart. He tells you he’s “been slowing down” a lot lately. He does not go down to the dining room because it is too taxing, he has been slowly losing weight because food does not taste good, he has fallen four times in the last year. He has no specific concerns to discuss today. What is the most important thing that can be addressed at today’s visit?
Test Questions Chapter 31
You have recently assumed directorship of a nursing home that has a 30-bed dementia unit. The nursing home does not have an onsite pharmacist. You go to the dementia unit for patient observation and chart review. Immediately, you notice that although it is 9:00 AM, and most of the patients have been taken out of their rooms and placed in the dayroom, they are dozing in their wheelchairs. The window blinds block about half of the sunlight, and without the overhead fluorescent lighting, the room would be considered dimly lit. The nurses have just finished administering the morning medications. You begin focused chart review, concentrating on patient medications, cognitive/functional status, and comorbidities. When you are finished, you note that of the 28 patients currently living in this facility, seven of them are receiving a low-moderate dose of an atypical antipsychotic (quetiapine, olanzapine, risperidone, etc.) before bedtime, but only one of these patients has any history of recurrent visual hallucinations and delusions. All of these individuals have either moderate-to-severe dementia from Alzheimer disease or vascular/Alzheimer overlay listed among their problems. You ask the charge nurse why these patients are receiving these medications, and he replies that his counterpart on the night shift stated that many of these patients did not sleep through the night, cried out from their rooms, woke other patients, and seriously disrupted the limited staff’s ability to manage the facility. The night nurse thus asked the previous attending to prescribe medications that would help these individuals sleep through the night.
- What further diagnostic steps are required in the seven patients receiving atypical antipsychotics?
- What is an appropriate step in the initial management of the seven patients receiving atypical antipsychotics?
- What aspects of sleep hygiene may make your facility more conducive for nighttime sleep?
- Which of the following statements regarding programs to increase daytime engagement in persons with dementia is true?
Test Questions Chapter 32
- What is the most common cause of erectile dysfunction in older men?
- Which is the most reasonable first step in the treatment of older men with erectile dysfunction?
- A 72-year-old woman reports vaginal dryness that interferes with coitus. Her medical history includes type 2 diabetes, hypertension, and osteoarthritis. Medications are glyburide, chlorthalidone, and acetaminophen. What would be your first step in therapy?
- A 70-year-old woman reports sexual pain with deep penetration only. What is the most likely cause of her problem?
Test Questions Chapter 33
- Subtypes of elder mistreatment include:
- Risk factors for elder mistreatment include all except:
- Barriers to detecting elder mistreatment include all except:
Test Questions Chapter 40
- An 85-year-old man with newly diagnosed nonvalvular atrial fibrillation comes to the office for a follow-up. He has a history of essential hypertension, type 2 diabetes mellitus, hyperlipidemia, and stage 3B chronic kidney disease. He takes lisinopril, atorvastatin, metformin, and aspirin. He lives in an assisted living facility and uses a walker for ambulation. He has fallen twice in the past year. On physical examination, his heart rate is normal but his rhythm is irregularly irregular. His blood pressure is 135/70 mmHg. Which medication change would be most appropriate for reducing his stroke risk?
- A 79-year-old woman was admitted to the hospital a month ago with an acute left middle cerebral artery ischemic stroke. On examination, she had right hemiparesis, mild motor aphasia, and dysphagia. After discharge, she was transferred to a skilled nursing facility where she has been working with physical, occupational, and speech therapy. Despite initial progress, in the last 2 weeks, she has lost her appetite, and complains of insomnia and difficulty concentrating. Which would be the next best step in management?
- An 82-year-old woman with a past medical history of essential hypertension and type 2 diabetes mellitus, and who currently smokes, was brought to the hospital after collapsing at home. The onset of her symptoms was 1 hour before arrival to the emergency room. On examination, she is awake, alert, and oriented to person, place, and time. She has moderate dysarthria, right gaze preference, left hemineglect, and left face, arm, and leg weakness. Her blood pressure is 190/90 mmHg and her glucose is 110 mg/dL. What diagnostic test should be done first?
Test Questions Chapter 46
- 1.A 79-year-old woman with a 1.5-cm breast cancer underwent lumpectomy. Pathology revealed ductal carcinoma that is hormone receptor negative (estrogen receptor 0%, progesterone receptor 1%) and HER2/neu negative. Surgical margins were adequate and uninvolved with cancer. Sentinel lymph node sampling was negative for lymph node involvement. She has good performance status and no activities of daily living (ADL) or instrumental (IADL) dependencies. What treatment would you recommend?
- An 86-year-old man with no ADL deficits who has stopped driving because of macular degeneration is evaluated for a urinary tract infection associated with urinary retention. The consulting urologist places a Foley catheter and sends a prostate-specific antigen (PSA) level that comes back 12 ng/mL. Three months later after the Foley has been removed and he has had a good response to tamsulosin, his PSA is still 10 ng/mL. What is the appropriate next step in managing this man’s prostate problem?
- In which of the following patients is chemical or surgical castration likely to prolong survival?
- On admission to the hospital, an 85-year-old woman was found to have a fungating mass on her right breast. The mass is 9 cm in diameter, partially ulcerated, and associated with edema of the arm and obvious pain. The patient has no children and had lived alone until recently, when a neighbor became concerned for what appeared to be a progressive loss of memory and neglect of the house. A nephew living in another city eventually came to take care of the situation and arranged for the admission. The patient appears confused and withdrawn; her appearance is disheveled, but she seems to be independent in her ADLs. The medical history is negative for any serious illnesses. She was able to drive her own car until shortly before this admission. The nephew does not wish to authorize hospice “right now.” A positron-emission tomography scan was negative for metastatic disease. In addition to determining the cause of her delirium, which of the following is the best way to address the breast mass?
- A 78-year-old man has an emergency partial colectomy for lower gastrointestinal bleeding. A localized colonic adenocarcinoma is completely resected. The surgeon did not dissect lymph nodes for metastatic sampling. The patient wants to know if he should have chemotherapy. Should he?
- An 80-year-old woman has no weight loss, no pain, and no distention but over 2 years increasingly complains of constipation despite adequate medical treatment. A colonoscopy is negative. An abdominal CT is performed. It reveals well-circumscribed pelvic masses, the largest adherent to the ovarian ligament. The best first step is:
Test Questions Chapter 49
- An 85-year-old man with chronic obstructive pulmonary disease presents to your office with his daughter with the complaint of new onset chest pain, shortness of breath, and cough. He is clearly tachypneic and has tactile fremitus and egophany and crackles heard at the right lung base. His daughter just wants you to give him an antibiotic pill so that she can take him home. You are concerned that he might need to be hospitalized and require IV antibiotics. What statement is true?
- An 80-year-old woman that you follow in a nursing home has an acute decline in her mental status. She has a fever >100° F, but no other focal complaints or findings on physical examination except for a chronic indwelling urinary catheter. What statement is true?
- An 82-year-old woman receives oral amoxicillin-clavulate for a skin abscess on her leg. She develops new onset of frequent watery stool that persists for several days after the antibiotic is stopped. You obtain a stool for Clostridium difficile antigen, toxin, and polymerase chain reaction (PCR). The antigen and PCR are both positive. She has never had C. difficile infection before. What one statement is the best answer regarding her management?
Test Questions Chapter 51
- A 75-year-old man presents with the chief concern, “I may have a bladder infection.” Further questioning reveals for several months he has been needing to void every couple of hours (can’t sit through a whole ball game), feels he must go as soon as he feels the urge (he tried putting it off and had urinary leakage), and is getting up two to three times at night to void. He denies delay in voiding or straining to initiate voiding, slow stream, feeling of incomplete emptying, or dribbling after completion of urination. He also denies dysuria and abdominal pain. Which of the following best describes the category or type of his lower urinary tract symptoms?
- A 70-year-old man has bothersome lower urinary tract syndrome (LUTS) associated with benign prostatic hyperplasia (BPH). His symptoms are no longer well managed with lifestyle modifications. He is interested in medication to reduce his urinary symptoms but is concerned about possible side effects. He notes that he is recently married and sexual activity is very important to him. Which of the following medications would be most appropriate for this patient?
- A 66-year-old man complains of nocturia (three to four times a night), hesitancy, and incomplete emptying of the bladder. Physical examination reveals an enlarged, nontender prostate, about 40 g in size without discrete nodules. Urinalysis reveals hematuria without leukocyte esterase. Upon further evaluation, the hematuria is attributed to his BPH. The patient declines surgical options at this time. Which of the following medications would be most appropriate?
- Mr. Quince is a 68-year-old patient who describes several months of urinary frequency and a sensation of incomplete emptying with no associated dysuria, hematuria, or fever. Physical examination reveals a slightly enlarged but nontender prostate, a postvoid residual urine volume of 20 mL, and a urinalysis with 15 white blood cells (WBCs) and 5 red blood cells (RBCs). Urine culture reveals 30,000 colony- forming units of Escherichia coli. You see a report from last year that shows urinalysis with 10 WBCs and 4 RBCs that was obtained as part of a routine evaluation. What is the most appropriate next step in the management of Mr. Quince’s symptoms?
- Mr. Roberts, a 72-year-old patient who has sought medical care on an intermittent basis in the past, complains of aching discomfort in his perineal area, urinary urgency, and frequency for the past few years. He also complains of insomnia and intermittent anxiety that he attributes to loneliness after his wife’s death about a year ago. Digital rectal examination (DRE) reveals a slightly enlarged, nontender prostate with no palpable nodules. Perineal examination is normal. Bladder scan is unremarkable and postvoid residual urine volume is 50 mL. Urinalysis shows no WBCs or RBCs. Urine culture is negative. Previous treatment has included dietary modification and alpha-blocker medication. What is the most appropriate next step?
- Mr. Hunter, a 69-year-old man, complains of urinary frequency and urgency that have increased over the past several months. There is no dysuria, hematuria, or sensation of incomplete voiding. He drinks 2 cups of coffee daily and diet cola multiple times a day. His International Prostate Symptom Score (IPSS) is 6, with a bother score of 1 indicating mild voiding symptoms with low impact on his quality of life. His medical history includes hypertension, coronary artery disease, and benign prostatic hyperplasia. Current medications are aspirin, metoprolol, and hydrochlorothiazide. Physical examination reveals normal sized prostate. Which of the following is the best next step?
- Two years later Mr. Hunter reports progression of his urinary symptoms and desires “a pill to make this better.” His current IPSS is 17, with a bother score of 3 indicating moderate voiding symptoms with moderate impact on his quality of life. On review of systems he notes that his vision has worsened, especially in his left eye. His ophthalmologist has recommended cataract surgery. For which of the following medications would initiation of therapy be delayed until after cataract surgery?
- Several years later, Mr. Hunter, who is now 75 years old, seeks additional intervention for his urinary symptoms that have progressed further. He now experiences slow urinary stream, hesitancy, straining, and a feeling of incomplete emptying in addition to the previous urinary urgency and frequency. At times, he has noted blood in his urine. He has had five urinary tract infections (UTIs) in the past 2 years. His current IPSS is 24, with a bother score of 5 indicating severe voiding symptoms with high impact on his quality of life……. Mr. Hunter’s updated medical history includes hypertension, coronary artery disease, benign prostatic hyperplasia, cataract surgery 4 years ago, and two falls within the past year while rushing to the bathroom during the night. Current medications are aspirin, metoprolol, finasteride, and tamsulosin. Physical examination reveals an enlarged, nontender prostate, about 50 g in size without discrete nodules. Upon further evaluation, the intermittent hematuria is attributed to BPH. Postvoid residual volume is 110 mL. Uroflowmetry reveals urinary flow rate of 12 mL/s. Which of the following is the best next step in management?
Test Questions Chapter 52
- A clinical prodrome of nonspecific symptoms of Parkinson disease (PD) include all the following except:
- The National Institute of Neurologic Disorders and Stroke (NINDS) criteria require a confirmatory autopsy for PD to be described as “definitive” but would rate as “probable” if three of the four primary clinical features were present for at least 3 years. Which of the following lists three primary clinical features of PD? (Choose one)
- Imaging plays a limited role in diagnoses of PD but is central in making diagnosis of:
- Key neurotransmitter-based therapeutic strategies for PD include all the following except:
- Treatment for early PD in an otherwise healthy older patient without significant functional impairment should begin with:
| Instituition / Term | |
| Term | Spring Term |
| Institution | Chamberlain |
| Contributor | Sharoon |