NR 601 Week 2 COPD Case Study - Part 1 (Initial post, Faculty and Peer Responses)
-
$15.00
| Institution | Chamberlain |
| Contributor | Chantara |
Purpose
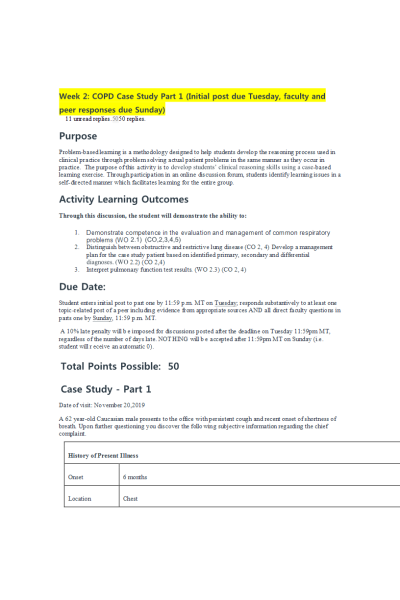
Problem-based learning is a methodology designed to help students develop the reasoning process used in clinical practice through problem solving actual patient problems in the same manner as they occur in practice. The purpose of this activity is to develop students’ clinical reasoning skills using a case-based learning exercise. Through participation in an online discussion forum, students identify learning issues in a self-directed manner which facilitates learning for the entire group.
A 10% late penalty will be imposed for discussions posted after the deadline on ..., regardless of the number of days late. NOTHING will be accepted after ... (i.e. student will receive an automatic 0).
Case Study - Part 1
A 62 year-old Caucasian male presents to the office with persistent cough and recent onset of shortness of breath. Upon further questioning you discover the following subjective information regarding the chief complaint.
| ||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||
Physical exam reveals the following:
| ||||||||||||||||||||
Requirements/Questions:
- Briefly and concisely summarize the history and physical (H&P) findings as if you were presenting it to your preceptor using the pertinent facts from the case. May use approved medical abbreviations. Avoid redundancy and irrelevant information.
- Provide a differential diagnosis (minimum of 3) which might explain the patient's chief complaint along with a brief statement (2-3 sentences) of pathophysiology for each.
- Analyze the differential by using the pertinent findings from the history and physical to argue for or against a diagnosis.
- Rank the differential in order of most likely to least likely.
- Identify any additional tests and/or procedures that you feel is necessary or needed to help you narrow your differential. All testing decisions must be supported with an evidence-based practice (EBP) argument as to why it is necessary or pertinent in this case. If no testing is indicated or needed, you must also support this decision with EBP evidence.
| Instituition / Term | |
| Term | Summer 2020 |
| Institution | Chamberlain |
| Contributor | Chantara |