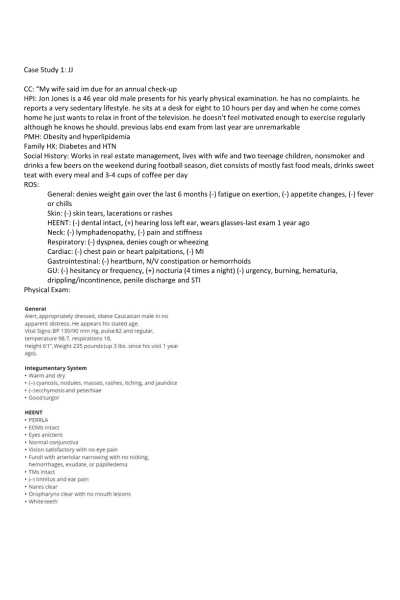
Case Study 1: JJ
CC: “My wife said im due for an annual check-up
HPI: Jon Jones is a 46 year old male presents for his yearly physical examination. he has no complaints. he reports a very sedentary lifestyle. he sits at a desk for eight to 10 hours per day and when he come comes home he just wants to relax in front of the television. he doesn't feel motivated enough to exercise regularly although he knows he should. previous labs end exam from last year are unremarkable
PMH: Obesity and hyperlipidemia
Family HX: Diabetes and HTN
Social History: Works in real estate management, lives with wife and two teenage children, nonsmoker and drinks a few beers on the weekend during football season, diet consists of mostly fast food meals, drinks sweet teat with every meal and 3-4 cups of coffee per day
ROS:
General: denies weight gain over the last 6 months (-) fatigue on exertion, (-) appetite changes, (-) fever or chills
Skin: (-) skin tears, lacerations or rashes
HEENT: (-) dental intact, (+) hearing loss left ear, wears glasses-last exam 1 year ago Neck: (-) lymphadenopathy, (-) pain and stiffness
Respiratory: (-) dyspnea, denies cough or wheezing Cardiac: (-) chest pain or heart palpitations, (-) MI
Gastrointestinal: (-) heartburn, N/V constipation or hemorrhoids
GU: (-) hesitancy or frequency, (+) nocturia (4 times a night) (-) urgency, burning, hematuria, drippling/incontinence, penile discharge and STI......... Continue
| Instituition / Term | |
| Term | Uploaded 2023 |
| Institution | Chamberlain |
| Contributor | |