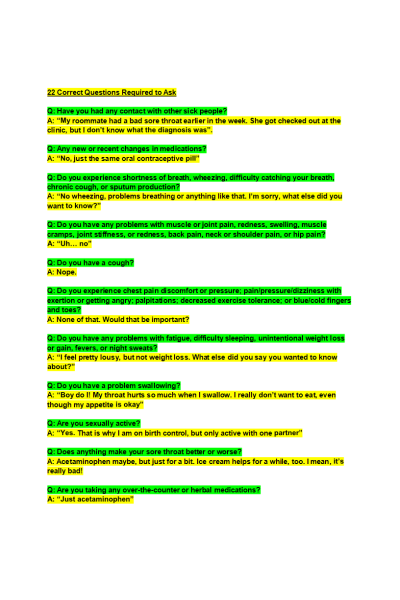
22 Correct Questions Required to Ask
Q: Have you had any contact with other sick people?
Q: Any new or recent changes in medications?
Q: Do you experience shortness of breath, wheezing, difficulty catching your breath, chronic cough, or sputum production?
Q: Do you have any problems with muscle or joint pain, redness, swelling, muscle cramps, joint stiffness, or redness, back pain, neck or shoulder pain, or hip pain?
Q: Do you experience chest pain discomfort or pressure; pain/pressure/dizziness with exertion or getting angry; palpitations; decreased exercise tolerance; or blue/cold fingers and toes?
Q: Do you have any problems with fatigue, difficulty sleeping, unintentional weight loss or gain, fevers, or night sweats?
Q: Do you have a problem swallowing?
Q: Are you sexually active?
Q: Does anything make your sore throat better or worse?
Q: Are you taking any over-the-counter or herbal medications?
Q: When did your sore throat start?
Q: Do you have chills? ......... Continue
Problem Statement (57 words long): JJ is a 23 year-old female with a history of infectious mononucleosis at age 15. She presents with acute onset of sore throat along with fever (101.8 F), bilaterally swollen lymph nodes that are tender to touch, headache, and difficulty swallowing. Patient symptoms began around 2 days ago following exposure to a sick roommate. Physical examination reveals fever of 101.5 F, bilateral cervical lymphadenopathy, erythema of the pharynx, and tonsillar exudate. Patient breathing is unlabored and clear to auscultation bilaterally. Patient taking acetaminophen as needed to reduce fever, headache, and sore throat symptoms. Cold food temporarily improves sore throat. Patient denies receiving flu vaccine this year. COVID series completed.
- name or initials, age
- chief complaint
- positive and negative subjective findings
- positive and negative objective findings
Key findings (7 listed by case):
MY FINDINGS
CASE FINDINGS
HISTORY OF PRESENT ILLNESS
Reason for Encounter:
History of Present Illness: The patient is a 23 y/o female who presents with acute sore throat which started around 2 days ago accompanied with fever of 101.8 F, headache, bilateral swelling of lymph nodes that are tender to touch, and difficulty swallowing. Patient experiencing ongoing discomfort from sore throat with minimal relief from acetaminophen and ice cream.
Patient also taking acetaminophen as needed to reduce fever and headache symptoms.
REVIEW OF SYSTEMS
- General:
- HEENT / Neck:
- Cardiovascular:
- Respiratory:
- Gastrointestinal:
- Genitourinary:.
- Musculoskeletal / Osteopathic Structural Examination:
- Neurologic:.
- Integumentary / Breast:
- Psychiatric:
- Endocrine:
- Hematologic / Lymphatic:
- Allergic / Immunologic:
PAST MEDICAL HISTORY
- Past Medical History:
- Hospitalizations / Surgeries:
- Preventative Health:
- Medications:
- Allergies:
- General:
- HEENT / NECK:
- Breast:
- Cardiovascular:
- Chest / Respiratory:
- Abdomen:
- Genitourinary / Rectal:
- Musculoskeletal / Osteopathic Structural Examination:
- Neurologic:
- Skin:
- Lymphatic:
- Psychiatric:
Please enter your assessment management plan and SOAP notes below:
Diagnosis: Pharyngitis, group A streptococcal
Diagnostic tests:
Medications:
Suggested consults/referrals:
Client education:
Follow-up, including time interval and specific symptomatology to prompt a sooner return. Provide rationales for each intervention and cite at least one relevant scholarly source as defined by program expectations:
| Instituition / Term | |
| Term | Uploaded 2023 |
| Institution | Chamberlain |
| Contributor | |