Prepare: Managing Patient Care
Nursing Care Delivery
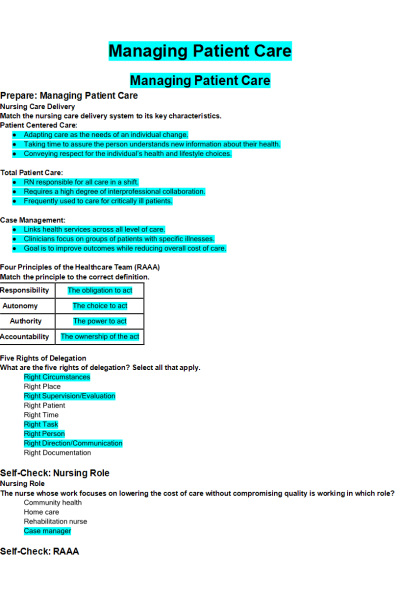
- Match the nursing care delivery system to its key characteristics.
- Patient Centered Care:
- Total Patient Care:
- Case Management:
Four Principles of the Healthcare Team (RAAA)
- Match the principle to the correct definition.
Five Rights of Delegation
- What are the five rights of delegation? Select all that apply.
Self-Check: Nursing Role
Nursing Role
- The nurse whose work focuses on lowering the cost of care without compromising quality is working in which role?
Self-Check: RAAA
RAAA
- For each situation indicate if the balance of responsibility, autonomy, authority, and are accountability is unequal by placing a check in the column associated with the factor that is out of balance. If the RAAA is balanced, place a check in the Balanced RAAA column. More than one factor may be affected in a situation.
Self-Check: Delegation and Maslow
Delegation
- For each instance of delegation, click to specify which of the five rights of delegation is being addressed. There may be multiple rights addressed for each example.
Self-Check: Interprofessional Communication
- Match the positive communication behavior to the category in which it falls.
- Value team input
- Exchange relevant information within the team
- Coordinate workload with colleagues
Self-Check: Knowledge for Nursing
Knowledge for Nursing
- The experienced nurse is precepting a nurse during their orientation to the facility. The orienting nurse has reviewed the policy and procedure manual for key nursing care activities and is preparing to bathe a patient with an indwelling urinary catheter. Before entering the patient’s room, the experienced nurse hands the orienting nurse packets of povidone-iodine (Betadine) swabs to cleanse the urinary catheter and perineum. The orienting nurse inquires if the patient has a condition that requires cleansing with something stronger than soap and water, which is what the facility policy and procedure manual recommends.
Both nurses reviewed the patient’s EHR and current procedure for catheter care to verify the correct type of catheter care was provided for this patient. What type of learning occurred in this situation?
Reflect: Managing Patient Care
Nursing Care Delivery Systems
- A patient who is critically ill will benefit most from being admitted to a nursing unit that utilizes which type of nursing care deliver system?
To Delegate, or Not to Delegate?
- Which aspects of nursing care should never be delegated to an unlicensed assistive personnel (UAP)? Select all that apply.
Nursing Attributes – Patient-Centered Care
- For each statement below, indicate if it reflects the definition of Patient-Centered Care (PCC), or an attribute of PCC Knowledge, PCC Skills, or PCC Attitudes by checking the correct box on the table. Note: Each statement will match only one column (Patient-Centered Care, Knowledge, Skills, or Attitudes).
Supervision While Delegating
- For each aspect of the Right Supervision/Evaluation step of delegation indicate who is responsible by placing a check in the Nurse or Unlicensed Assistive Personnel (UAP) column. Each aspect may apply to both colleagues.
Imbalance of RAAA in Conversation
- The nurse is caring for an elderly client who is cooperative and pleasant. About two hours into the shift the client says, “You are so pretty and could be beautiful if you did not have acne.” The nurse thanks her for the compliment, finishes administering medications, assures the client has what she needs, and leaves the room. Over the next several hours the client continues to comment on the nurse’s acne, despite the nurse’s request that she not. When the nurse realizes their emotions may interfere with their care of the client, they speak with their nurse manager and the client is assigned to another nurse for the remainder of the shift.
In the table below, place a check to indicate which factor is imbalanced in this communication. If all factors are balanced, place a check in Balanced RAAA.
Unexpected Discovery
- The nurse asks an Unlicensed Assistive Personnel (UAP) to total the shift intake and output for a group of patients to which the UAP is not assigned. After clarifying the nurse’s expectations related to time of completion and reporting back, the UAP enters the room of a patient with IV fluids infusing. The Intake and Output Record does not include an intake amount for IV fluids, though. What should the UAP do?
RAAA in Action
- The nurse is caring for a patient experiencing an extremely low blood pressure. The health care provider prescribes a vasoconstrictive medication with which the nurse is unfamiliar. When considering which action to take next, the nurse considers which aspects of RAAA? Select all that apply.
Delegation
- Four hours after delegating the task of taking a patient’s vital signs to an Unlicensed Assistive Personnel (UAP) colleague, the nurse notes in the documentation that the blood pressure reading was dangerously high. The nurse approaches the UAP and lectures them for not reporting the abnormal reading immediately. The UAP tells the nurse that it is not their job to make sure the nurses look at the chart.
Determine if the Nurse and/or the UAP properly incorporated RAAA and the Five Rights of Delegation into their actions by dragging Nurse and/or UAP to the correct column. Remember, it can be either the Nurse, the UAP, or both for each row.
Clinical Care Coordination
Prepare: Clinical Care Coordination
Shared Leadership Characteristics
- Indicate which leadership characteristics are required of the nurse leader and which are required by the staff nurse by placing a check in the appropriate column. Note, some characteristics may apply to both.
Value of Clinical Decisions
- The nurse uses clinical decision making to keep the health care team focused on actions that move the client toward health.
Client’s Valuables
- When admitting a client to an acute care facility (hospital), the nurse addresses safe keeping of the client’s belongings. Place the actions in the order in which the nurse completes them, starting with the first.
Self-Check: Keys to Good Clinical Decisions
- Which factors increase the quality of clinical decisions made by the nurse? Select all that apply.
Self-Check: Working Smart
Working Smart
- The nurse assessing a client’s foot wound is unsure if the underlying cause is related to arterial or venous insufficiency. Realizing that the plan of care will differ based on the underlying pathology, what is the best action for the nurse to take?
Self-Check: Sorting Priorities
- Sort the interventions based on the level of priority: time dependent, client needs, or client preference.
- Time Dependent Priorities
- Client Needs Priorities
- Client Preference Priorities
Self-Check: Change of Plans
- After caring for a client on the first day of a two-day clinical, the student nurse was confident that the schedule for the second day would be exactly how their time together would be. Listen to the report given to the student by the nurse, then drag the items for the new plan to correct times in the New Plan column.
Self-Check: Patient Belongings
Patient Belongings
- Mr. Smith, recovering from a stroke, asks the nurse where his wallet is and says he is worried about his credit cards and the $64 in cash he had when he was first admitted. After looking around the room, in drawers and through his clothing without locating the wallet, the nurse checks the valuables inventory completed when Mr. Smith was admitted. What is the best response by the nurse after seeing this information in the EHR?
“According to the admission valuables inventory you did not have a wallet or cash when you arrived. You did have a watch and ring that was sent home with your son, though. Is it possible he also has your wallet?”
“Well, the chart says you did not have any cash. Could you be mistaken?”
“Based on what I see in your record, you did not have any cash or a wallet when you were admitted. Do you want me to contact security so you can make a missing property report?”
“Things go missing in the hospital, unfortunately. Do you know if your wallet was with your belongings before you had your MRI two days ago?
Reflect: Clinical Care Coordination
Prioritizing Assessment Findings
- After the nurse has performed a skin assessment on a recently admitted 19-year-old client, which finding is the highest priority to report to the healthcare provider?
Prioritizing Client Needs
- After the nurse receives change-of-shift report, which client should be assessed first?
Appropriate Teamwork
- The nurse is caring for a client with osteoporosis who is at increased risk for falls. Which intervention should the nurse delegate to the unlicensed assistive personnel (UAP)?
Prioritizing Care of Medication Error
- The nurse is supervising a practical nurse (PN) who says, “I gave the client with myasthenia gravis 90 mg of neostigmine instead of the ordered 45 mg!” In which order should the nurse perform the following actions?
Clinical Decision Making & Priorities
- The nurse has completed passing medications to a stable client on airborne precautions and is preparing to provide education on new medications. A Rapid Response Team is paged to the room of another one of the nurse's clients. Before leaving the client’s room, list the steps the nurse will take in the correct order, starting with the first.
Aspects of Clinical Care Coordination
- In the table below, match the items in student, linking phrase, and nurse columns.
Securing Client Valuables
- A client who was admitted after a motor vehicle crash is scheduled for surgery later in the day. When completing a focused assessment, the nurse notices that the client is wearing a wedding band and has a mobile phone with a charging plug/cable, and their wallet, dentures, and a case for their contact lenses are sitting on the bedside table.
Drag each of the client’s possessions to the cells on the table that indicate the appropriate level of security and storage for each item.
Ranking Priorities
- It is 23:30 and the oncoming nurse is determining the order in which to see their clients. Place these clients in the order in which the nurse should see them, with first on top and last on the bottom.
Ethics of Patient Care
Prepare: Ethics and Morals
Ethics in Action
- What steps can the nurse take to assure a new client understands their rights and responsibilities related to receiving healthcare? Select all that apply.
Ethics and Morals
- In its simplest form, a moral describes the value an individual or group attaches to right and wrong. It is these values, or morals, that influence not only their own behavior but how they interpret the behavior of others. Ethics is the study of right and wrong applied to questions of correct behavior. Behavior is interpreted as responsible or irresponsible when judged against agreed-upon aspects of universal fairness. In theory, ethical principles apply to all actions equally.
Ethics and Protected Health Information (PHI)
- A woman calls the hospital asking for information on a client’s condition. She claims to be the client’s ex-wife and demands to speak with the healthcare provider about the current treatment plan. The nurse explains that they are unable to speak to her because her name is not included on a list of persons with whom the client’s information can be shared.
Self-Check: Ethical Principles
Ethical Principles
- For each situation, select the ethical principle that is involved using the drop down menu.
Self-Check: Resolving an Ethical Dilemma
Resolving an Ethical Dilemma
- Place the key steps for ethical dilemma resolution in the correct order, starting with the first and ending with the last.
Self-Check: Right to Refuse Care: Bill
Right to Refuse Care: Bill
- Bill, a college graduate in his mid-twenties, was brought to the emergency department (ED) by friends after experiencing chest pain that radiated to his neck and left arm. After initial assessment and testing that determined the pain was angina, rather than a myocardial infarction (MI), admission to the hospital for observation and further testing was recommended. Since he has no medical insurance, Bill refused to be admitted and promised to follow up at a nearby clinic for care. Place the nurse’s responsibilities involved with Bill’s refusal to provide care in order, starting with the first and ending with the last.
Explore: Healthcare Specific Ethical Concerns
Healthcare Specific Ethical Concerns
- A nurse, whose grandfather recently passed away, is returning to work after bereavement leave and learns during report that one of their assigned clients is at the end of their life. The nurse believes they will be unable to provide care for this client and family due to their emotions. What is the best action for the nurse to take?
Self-Check: Benefits of Social Media Guidelines in Health Care
- For each social media guideline, indicate if it protects the client, the nurse, or the organization by placing a check mark in the corresponding column.
Reflect: Ethics of Patient Care
Obtaining a Signature on a Surgical Consent Form
- Based on the documentation below, what action/actions will the nurse take next? Select all that apply.
Privacy Wanted
- The nurse sitting at the nurses’ station is preparing to call a client’s health care provider to report a change in their condition. For each area marked, use the drop down menus to indicate if it presents a risk to the client’s privacy and confidentiality by selecting Risk or No Risk.
Advocating for Client Autonomy
- A client who does not want to have their life prolonged by artificial means, including CPR, shares with the nurse that they are concerned their family will not accept their wishes. How does the nurse act as an advocate for this client? Select all that apply.
Responding to an Ethical Dilemma
- The nurse is caring for a client admitted with a gun shot wound to the left thorax that resulted in fractured ribs and a hemopneumothorax. The client has requested that their name not be listed on the list of individuals currently in the hospital as they believe they are in danger, though they do not know who shot them. A woman who identified as the client’s daughter is calling for an update on the client. In what order will the nurse complete these actions? Place actions in order, from first to last
Applying Ethical Principles
- The nurse is caring for a client admitted with a gun shot wound to the left thorax that resulted in fractured ribs and a hemopneumothorax. The client has requested that their name not be listed on the list of individuals currently in the hospital as they believe they are in danger, though they do not know who shot them. The nurse complies with the request and, with the permission of the client, approaches the 16 family members who are in the visitor’s lounge waiting to see their loved one while the client’s partner stays at the bedside. During the discussion with the family, the eldest daughter pulls the nurse aside and states that they believe the client was shot by his partner during a domestic dispute. The nurse returns to the client’s bedside, asks the partner to leave, assesses the client’s safety status and discovers imminent danger. Based on this interaction, the nurse explains to the client that they are mandated to follow hospital policy and share this information with the nursing supervisor and security
Accessibility Planning
- The nurse is providing discharge teaching to a client who has recently lost the use of their legs and is now mobile in a wheelchair. The client and their partner show the nurse a picture of their bathroom and ask for input on what items need to be changed to promote the client’s self-care autonomy. Using the drop-down menus, indicate if the item needs to be updated or can be left as is.
Identify Reason for Seeking Care
A nurse arrives at work and is told to report to the intensive care unit (ICU) for the day due to short staffing. The nurse has never worked in the ICU. Which is the most appropriate action by the nurse?
Social Media and the Nurse
- The nurse caring for a friend who is ready to be discharged home after surgery takes a picture with the friend as she sits in the car and posts it on social media with the caption, “So proud of my BFF for being the best client ever! Love you!!!❤” Which ethical or professional standards (left column below) has the nurse violated or not violated? Select all that apply
Legal Aspects of Providing Care
Prepare: Legal Aspects of Providing Care
Living Will
- The nurse notes that a living will is in the client's medical record. Which of the following statements represents the best description of guidelines a nurse would follow in this case?
Types of Law
- Match the definition below with the type of law it describes:
Consent for Minors
- Ordinarily minors may not consent to medical treatment for themselves. The nurse understands that this does not apply to emancipated minors and unemancipated minors in certain situations. For each situation listed, indicate if consent can be provided by an emancipated or unemancipated minor by placing a check in the appropriate column.
Self-Check: Torts in Healthcare
Torts in Healthcare
- For each situation, use the first drop down menu to indicate if the actions involved were intentional, quasiintentional, or unintentional. Use the second drop down menu to indicate which tort was committed.
The unlicensed assistive personnel (UAP) tells a school-aged client who is not cooperating at bedtime that the nurse will give them a shot if they don’t behave.
- The nurse caring for an elderly client in a residential memory care facility is concerned that Mrs. Baxter is at risk of malnourishment because she will not sit down long enough to eat her meals. The nurse seats Mrs. Baxter in a wheelchair with the brakes engaged at the table during lunch. After 5 minutes, Mrs. Baxter wants to leave the dining room. The nurse knows that the patient is unable to unlock the wheelchair and ignores the request because she wants the client to sit long enough to eat her meal.
- When administering medications, the nurse knocks on the door to the client’s room and enters without waiting for permission. The client is standing beside the bed urinating in full view of people in the hallway.
- The nurse exits the client’s room, who is on complete bedrest, without placing the phone within reach. When the nurse returns to the room, the client is lying on the floor and explains that they didn’t want to bother the nurse and fell trying to reach for the phone.
Self-Check: Providing Unwanted Care
Providing Unwanted Care
- Although the client refused the procedure, the nurse insisted and inserted a nasogastric tube in the right nostril. This is an example of battery which is an intentional tort.
Self-Check: Components of Informed Consent
- Informed consent is an agreement from the client to have a medical procedure and requires full disclosure of the risks and benefits of treatment, alternative care options, and the consequences of taking no action from the healthcare provider. The information provided to obtain consent must be done using terms that the client understands. Elements of informed consent: diagnosis and purpose of proposed action; risks and benefits of action, alternatives (regardless of cost or insurance), risks and benefits of alternatives, risks and benefits of no action. It also requires that the client has the capacity to understand your options for care.
Self-Check: Patient Self-Determination Act
- A middle-aged adult presents to the clinic for follow-up after having been diagnosed with pulmonary hypertension. The client works as a local politician and has a history of sarcoidosis. Their vital signs are within normal reference ranges. The client states that they wish to discuss options for care as their conditions worsen. Which provision of the Patient Self-Determination Act (PSDA) requires health professionals participate in this discussion?
Self-Check: DNR: Roles and Responsibilities
- For each action associated with enacting a Do Not Resuscitate Order (DNR), indicate which individual is responsible for completion by placing a check in the appropriate column or columns. Select all that apply for each action.
Reflect: Legal Aspects of Providing Care
Scope of Practice and the Law
- Which actions by the nurse could result in both criminal and civil law sanctions? Select all that apply.
Malpractice
- Separate these nursing actions based on whether or not it could result in the nurse being found liable of malpractice by dragging the sentence to the correct location.
Breach of Duty
- A client has a fractured femur that is placed in skeletal traction with a fresh plaster cast applied. The client experiences decreased sensation and a cold feeling in the toes of the affected leg. The nurse observes that the client's toes have become pale and cold but forgets to document this because one of the nurse's other clients experienced cardiac arrest at the same time. Two days later the client in skeletal traction has an elevated temperature, and he is prepared for surgery to amputate the leg below the knee. Which statements regarding a breach of duty apply to this situation? Select all that apply.
Living Will and Durable Power of Attorney for Health Care
- For each client described below, indicate if a durable power of attorney for healthcare (DPOA) or living will is recommended by placing a check in the appropriate column or columns. Select one or both for each client.
Reporting Abuse
- While assessing a newborn client discharged from the neonatal intensive care unit the previous day, a home health nurse notices significant bruising on the 2-year-old sibling’s head, arms, abdomen, and legs who is wearing only a diaper and playing with age appropriate toys. The parent of both children describes the toddler as “quite clumsy” and “always running into things” before handing the newborn to the nurse.
Place the actions the nurse will take, in the order in which they should be completed, starting with the first.
Supporting Client Self-Determination
- An older adult presents to the clinic with their adult daughter. After the physical examination is completed, the client asks to speak with the nurse in private. Once alone, the client explains that the daughter dictates their healthcarerelated decisions regarding medications, sometimes against their wishes. The client asks if they have any legal rights to assure they are able to make healthcare decisions for themselves. What information will the nurse provide? Select all that apply.
Helping Others in an Emergency
- The nurse stops at the scene of a motor vehicle crash intending to assist individuals who were injured. The nurse understands their actions are supported by which principles? Select all that apply.
Identifying Malpractice
- A healthcare provider prescribes one tablet of a medication, but the nurse accidentally administers two. The nurse monitors the client for untoward effects of which there are none, then notifies the healthcare provider. Is the client likely to be successful in suing the nurse for malpractice?
Nursing Application for Managing Patient Care
Prepare: Nursing Application: Nursing Application: Managing Patient Care
Scope of Practice
- Which actions are appropriate to assign to a practical nurse (PN) working under the supervision of a registered nurse (RN)? Select all that apply.
Supervision
- A client with an expected outcome of “Able to bathe and brush teeth independently” is looking forward to discharge in the near future. The nurse observes the unlicensed assistive personnel (UAP) performing these actions. For which action must the nurse intervene?
Prioritizing in an Emergency
- The nurse and their family are at the lake with friends. During lunch, the nurse’s partner says, “Look to the left about 50 feet out, I think someone is drowning!” Place the following nursing actions in an order of priority:
Self-Check: The Case of Susan M.
Recognizing Cues - Susan M.
- Susan M. is an 82-year-old retired school teacher living with vascular dementia. Her son Rich moved into her home to care for Susan 18 months ago. Today, Rich has brought Susan to the emergency department due to increased confusion. A nurse assigned to complete Susan’s initial assessment, creating the nursing plan of care, and care for her during the shift.
Select the words or phrases in the son’s reason for admission that alert the nurse to seek additional information related to the relationship between Richard and his mother.
Forming Hypotheses - Susan M.
- Based on priority assessment cues, on which hypotheses will the nurse base follow-up questions? Drag the 3 priority hypotheses to the target location.
Physical Assessment – Susan M.
- Based on the priority cues discovered about Susan, use a nursing diagnosis text to select the highest priority hypothesis suggested by the current cues, the top 2 actions the nurse will take to gather more data related to that diagnosis, and the top 2 findings that support that diagnosis.
Documentation of Assessment Findings - Susan M.
- When documenting Susan’s complete assessment, what information related to caregiver role strain will the nurse include in the electronic health record (EHR)? Select all that apply.
Delegation of Care - Susan M.
- For each client care activity planned for Susan, indicate which nursing colleague, registered nurse (RN), practical nurse (PN), and/or unlicensed assistive personnel (UAP) can complete the action.
Reflect: Nursing Application: Managing Patient Care
Prioritizing Nursing Actions - Johnny Rokeby
- Review the electronic health record before answering each question. For which order, or orders, will the nurse contact the health care provider prior to taking action? Select all that apply.
Sequence of Nursing Actions - Johnny Rokeby
- Place the actions in the order in which the nurse will perform them, starting with the first and ending with the last.
Responding to Interruption - Johnny Rokeby
- The nurse has entered Johnny’s room to insert the peripheral venous access device, initiate intravenous (IV) fluids, and start the antibiotic. While organizing the equipment and explaining what is being done, the nurse receives a request from another client to assist them with required ambulation. The client is stable and practicing walking with crutches prior to discharge in a few hours. Nursing colleagues available to assist the client include two registered nurses (RNs), one practical nurse (PN), and one unlicensed assistive personnel (UAP). What is the best action for the RN to take?
Overheard - Johnny Rokeby
- The nurse is approached by Johnny’s oldest daughter, Cecilia, who is concerned about her father’s privacy after overhearing one of the other nurses from this unit talking with colleagues about her father having been admitted. What is the best response by the nurse?
Breach of Duty - Johnny Rokeby
- After returning from lunch, the nurse is reviewing Johnny’s electronic health record (EHR) and sees that another nurse has administered medications. Select the item below that needs immediate action.
Do Not Resuscitate Order - Johnny Rokeby
- Three days after admission Johnny’s pneumonia worsens and he becomes septic. He has been intubated and transferred to the intensive care unit (ICU) where he remains unresponsive, breathing only with the assistance of the ventilator, and receiving medications to keep his blood pressure near normal. Because Johnny had a living will document that indicated he would not want to be kept alive in these conditions, the family approaches the nurse about enacting his living will document so the life support measures can be stopped. What information does the nurse provide to inform the family of what will happen next?
Recognizing Cues - Johnny Rokeby
- The nurse discontinued the ventilator and suctioned the endotracheal tube in anticipation of extubation but noticed a potential improvement in his condition. Which cues indicate that Johnny’s condition is improving? Select all that apply.
- As Johnny’s condition begins to improve, his daughter asks if the do not resuscitate (DNR) order can be canceled. What is the best response by the nurse.
| Instituition / Term | |
| Term | Uploaded 2023 |
| Institution | Chamberlain |
| Contributor | Amelia |